The role of hyperbaric oxygen in the treatment of intestinal obstruction
The role of hyperbaric oxygen in the treatment of intestinal obstruction
Intestinal obstruction refers to the obstruction of the contents in the intestines. It is a common acute disease. If handled improperly there will be the risk of death. The mortality rate is about 5%-10%.
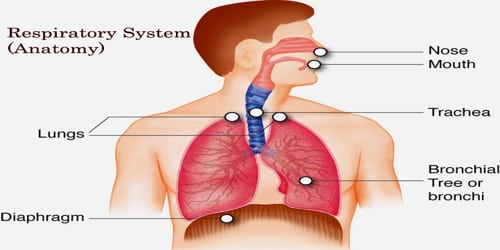
Paralytic intestinal obstruction and adhesive intestinal obstruction are common complications after major abdominal surgery. Clinically, gastrointestinal decompression, drugs or surgery are generally used. As a safe and non-invasive treatment, hyperbaric oxygen technology has been continuously applied to the prevention and treatment of postoperative intestinal obstruction.
Mechanism of hyperbaric oxygen treatment of paralytic intestinal obstruction
- In the state of hyperbaric oxygen, the volume of gas in the intestinal obstruction cavity reduces, the pressure in the cavity relieves, restores the intestinal tract to normal, then improves the blood supply of the intestinal wall, thereby accelerating the absorption of gas.
- Hyperbaric oxygen can rapidly increase the partial pressure of oxygen in the blood and intestinal wall tissues and improve oxygen supply.
- The intestinal wall vasoconstriction can reduce vascular exudation, reduce edema, and accelerate the recovery of intestinal peristalsis.
- Hyperbaric oxygen also helps prevent and control secondary infections in the diseased bowel.
Related research
Among the 133 cases of abdominal surgery patients who were observed preventive use of hyperbaric oxygen therapy, only 3 patients developed paralytic intestinal obstruction and adhesive intestinal obstruction. After comprehensive treatment such as hyperbaric oxygen chambers, the symptoms gradually disappeared. In another group of 199 patients who did not use hyperbaric oxygen therapy for abdominal surgery, 9 patients had postoperative paralytic intestinal obstruction and adhesive intestinal obstruction, and 2 of them underwent adhesion lysis due to conservative ineffectiveness. Patients who were given preventive hyperbaric oxygen therapy had significantly shorter hospital stays after surgery than patients who were not initially given hyperbaric oxygen therapy.
Another retrospective study found that the total effective rates of patients with postoperative paralytic intestinal obstruction and adhesive intestinal obstruction after receiving hyperbaric oxygen therapy were 92% and 85%, respectively.
Studies have shown that hyperbaric oxygen therapy has the potential to prevent postoperative paralytic intestinal obstruction and secondary adhesion, and it has a good therapeutic effect for patients with early postoperative recurrent adhesive intestinal obstruction to relieve adhesion. Patients who received hyperbaric oxygen therapy as the treatment of early recurrence of intestinal obstruction had a significantly shorter hospital stay than patients with conservative treatments. It can minimize the suffering and burden of patients, reduce medical expenses, and help improve their quality of life.