Our experience: Can hyperbaric oxygen therapy work for fibromyalgia?
Hyperbaric oxygen & Fibromyalgia
Fibromyalgia is characterized by chronic pain at multiple specific anatomic sites lasting more than 3 months and is often accompanied by clinical manifestations such as fatigue, muscle and joint stiffness, sleep disturbances, irritable bowel syndrome, weakness and fatigue, cognitive impairment, and depressive symptoms.
Fibromyalgia affects women more, with an estimated 2% to 8% of the world's population suffering from it. Fibromyalgia usually appears in the age range of 30 to 35 years. The quality of life of people with fibromyalgia is severely impaired and can lead to suicide associated with depression and worsening mental status.
Today's English literature is a case report about a fibromyalgia patient who experienced significant improvement in clinical symptoms after 40 sessions of hyperbaric oxygen therapy, and all symptom areas reported before treatment were improved.
References: Garlı M, Küsbeci T, Aydın F, et al. The effect of hyperbaric oxygen therapy on corneal endothelial structure and anterior segment parameters. Cutan Ocul Toxicol. 2023 Aug 9:1-5.
Patient situation
In January 2021, a 54-year-old woman with a negative history reported pain in her left arm 24 hours after receiving her first dose of Pfizer vaccine. Local pain at the injection site (left triceps) accompanied by high fever (40 ° C), severe headache, vomiting and abdominal pain. After 48 hours, the fever began to return to normal temperature, but fatigue gradually appeared.
Subsequently, the patient reported pain relief in the left arm, persistent, severe, and persistent pain in the occipital and dorsal-neck regions, lower back, and legs, and significant lower extremity gravity. The patient also complained of difficulty walking on foot and the need to use crutches. In addition, she reported stiff facial muscles, pain defined as intense, mental ambiguity, severe short-term memory impairment, and progressive depression, symptoms that undoubtedly took a serious toll on her quality of life.
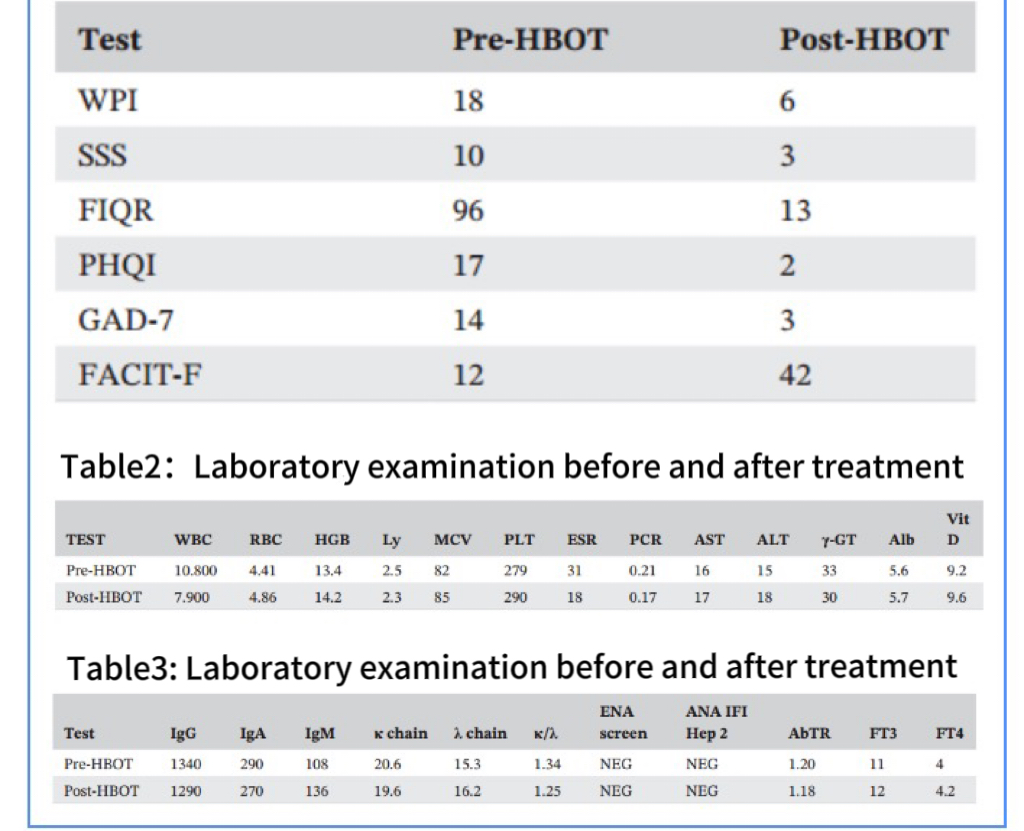
Patients underwent routine blood tests (blood count, ESR, polymerase chain reaction, protein electrophoresis, aspartate aminotransferase, alanine aminotransferase) and more specific immunoenzyme tests (serum kappa and lambda chains, IgG, IgA, IgM, antinuclear antibodies, ENA, and ANA subclasses).
In addition, tests were performed to rule out the presence of viral hepatitis and functional thyroid lesions (TSH, FT3, FT4, anti-thyroglobulin, and anti-thyroid peroxidase antibodies), which proved negative.
Check that no values outside the standard range are displayed. There was only a slight increase in ESR and a slight decrease in 25-hydroxyvitamin D levels. The patient also underwent whole-body CT, spinal MRI, and bone density measurements of the femur and lumbar vertebra, which revealed no prominent structural morphological changes other than initial photographs of osteoporosis consistent with the patient's postmenopausal age. The exclusion of inflammatory diseases, although some rheumatic diseases can coexist, suggests a possible diagnosis of fibromyalgia, so rheumatologists seek its diagnostic criteria. The pain lasted longer than 3 months (patients reported symptoms appearing about 18 months ago).
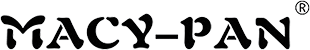
The Generalized Pain Index (WPI), Symptom Severity Scale (SSS), revised Fibromyalgia Impact Questionnaire (FIQR), Pittsburgh Sleep Quality Index (PHQI), Generalized Anxiety Disorder Screening Scale (GAD-7), and Chronic Disease Treatment Fatigue Function Rating Scale (Facit-F) were used.
The scores of the questionnaire conducted before the start of hyperbaric oxygen were as follows: WPI=18, SSS=10, FIQR=96, PHQI=17, GAD-7=14, Facit=12.
So she began a multidisciplinary treatment process based on pain therapy, physical therapy, psychological support, relaxation techniques and healthy nutrition.
HBOT
Among the various therapies, hyperbaric oxygen is considered an experimental and unconventional treatment.
Hyperbaric oxygen therapy: 2.4ATA, stabilized oxygen for 60 minutes, once a day, 5 times a week. Treatment will begin in the first week of September and end in mid-November 2022, with a total of 40 treatments.
improvement of symptoms
clinical manifestation
During each session, patients showed stable vital parameters (blood pressure, heart rate, oxygen saturation, and body temperature). Blood tests, markers of periodontitis and blood chemistry performed during the middle and end of treatment showed that the values did not exceed the normal range.
The patients received 40 sessions of hyperbaric oxygen therapy. Clinically, the improvement achieved was significant, with improvements in all symptom areas reported prior to treatment. In particular, full recovery of mobility, absence of crutches, increased muscle strength, ability to climb several flights of stairs and walk long distances independently.
This patient reported a significant reduction in pain symptoms from the moment she woke up in the morning, a significant improvement in sleep quality that had previously been reported as mild, non-restorative, and with multiple intervals. It is reported that highly debilitating fatigue is significantly reduced after treatment and is easy to deal with anyway.
In addition, significant changes in cognitive abilities were reported, mental ambiguity disappeared, and short-term memory was restored. All in all, there was a significant improvement in quality of life as the depression in which the patient had fallen disappeared, a situation confirmed by psychological counseling at the end of the high-pressure treatment.
Laboratory examination or evaluation score
Table 1: Generalized Pain Index (WPI), Symptom Severity Scale (SSS), Revised Fibromyalgia Impact Questionnaire (FIQR), Pittsburgh Sleep Quality Index (PHQI), Generalized Anxiety Disorder Screening (GAD-7), and chronic Disease Treatment Fatigue Function Assessment (Facit-F).

Fibromyalgia is a central sensitization syndrome that involves dysfunction of neural circuits involved in the perception, transmission, and processing of injurious afferents. Pain is mainly manifested in the musculoskeletal system. It is an incurable disease of unknown cause, and its signs and symptoms often resemble or overlap with other syndromes. Unfortunately, this happens with a high frequency, delaying diagnosis. The pathogenesis of clinical manifestations is the change of the nociceptive system.
The hypothesis that reduced oxygen supply may be the cause of muscle structural and functional degeneration affecting fibromyalgia patients dates back to the first half of the 1970s. Several studies have shown that in fibromyalgia patients, reduced oxygen availability, both absolute and associated with low tissue extraction fractions, leads to low perfusion/ischemia, which in turn may play a key role in the occurrence of muscle pain, a prominent feature of the clinical characteristics of patients with fibromyalgia.
Subsequently, to clarify the pathogenesis of fibromyalgia produced an endless number of research results, and put forward some views. Environmental, psychosocial and genetic aspects are thought to contribute to a reduced tolerance for adverse stressful events, which appears to make these individuals more vulnerable.
It is speculated that environmental factors such as adverse events that occur early in life, psychosocial stress, trauma, and medical conditions (e.g., Lyme disease, Epstein-Barr virus infection, viral hepatitis, Q fever) can trigger the development of fibromyalgia.
Another study involved thalamic mast cells, which appear to play a role in the development of inflammation and pain by releasing pro-inflammatory mediators (interleukin alpha, tumor necrosis factor-alpha) and by stimulating nociceptor neurons in the thalamus through direct and indirect pathways. Trauma and infection often precede the onset of fibromyalgia, suggesting a potential role for immunomodulatory pathways. Another interesting theory being evaluated suggests changes in serum levels of certain neurotransmitters (serine and glutamate), which in turn are associated with gut-brain crosstalk. Multiple studies have suggested that reduced levels of bioamines, impaired regulation of the hypothalamic-pituitary axis, and increased concentrations of excitatory neuromolecules (especially substance P) may play a central role in the onset of the clinical model.
Until now, dysfunction of the neural circuits involved in the perception, transmission, and processing of injurious afference has been considered a key factor in the occurrence of fibromyalgia symptoms, and in fact, some studies have shown that damage to the neurotransmitter system can affect pain perception, fatigue, sleep disturbances, anxiety symptoms, and depression. People with fibromyalgia show high levels of norepinephrine and glutamate and low levels of serotonin and dopamine. As mentioned above, Substance P levels in the cerebrospinal fluid of fibromyalgia patients are three times higher than in healthy people.
The extreme variety of symptoms and associated comorbidities make the diagnosis of fibromyalgia problematic. Fibromyalgia is often observed in connection with other conditions, such as osteoarthritis, rheumatoid arthritis, and lupus. Many doctors are unfamiliar with the diagnostic criteria, have no clinical experience with these patients, and are unaware of potential treatment options.
As described by Choy et al., a diagnosis resulting from these factors typically takes more than two years and involves an average of 3.7 physicians per patient. Clearly, early diagnosis of fibromyalgia is crucial to avoid the worsening of initial symptoms and the development of a vicious cycle, such as pain with immobility and/or pain with mood disorders, which can further complicate the treatment of these patients. The diagnostic criteria for fibromyalgia evolved from pioneering work by the American College of Rheumatology (ACR) to a critical review published by the same authors in 2016, which is now considered a reference point for the diagnosis of fibromyalgia. In short, diagnosis is based on the discovery of the following clinical symptoms:
1.WPI≥7 points and SSS≥5 points; Or WPI 4-6 points and SSS≥9 points.
- Generalized pain, present in at least four of the five defined location areas.
- Symptoms must have been prevalent for at least 3 months.
The five defined location regions considered are defined as the upper right and upper left regions, lower right and lower left regions, and central axis regions. Some authors have recently suggested that patients should be screened for WPI and further screened for the main symptoms of fibromyalgia in WPI-positive patients according to ACR's 2016 criteria.
Unfortunately, to date, there is no universally accepted effective treatment, treatment is multidisciplinary, and as a result, different treatment puzzles focus on controlling and managing pain symptoms. Treatment is based on a combination of different classes of medications (antidepressants, anticonvulsants, muscle relaxants, painkillers, hypnotics, antipsychotics, cannabis and cannabinoids) and non-pharmacological therapies such as fitness, psychotherapy, hydrotherapy, tai chi, qigong, yoga, mindfulness, hypnosis, acupuncture, heat and electricity. In fact, their combined use has been shown to relieve pain, with variable and time-limited benefits.
In a clinical setting, the pressure applied by a hyperbaric oxygen chamber is usually between 2 and 3ATA. In patients with normal pulmonary function and normal arterial blood flow at high atmospheric pressure, the alveolar oxygen partial pressure (PaO2) increases significantly, proportional to atmospheric pressure, to 1500 and 200 mm Hg at 2ATA, respectively.
Hyperbaric oxygen is based on several physiological principles related to the response of gases to pressure and, more precisely, the response of oxygen to pressure. In fact, the concentration of dissolved oxygen in plasma can be strongly affected by hyperbaric oxygen. According to Henry's law, an increase in pressure causes more gas to enter the solution, so more oxygen is brought to the plasma. As defined by Fick's law, an increase in partial pressure increases the driving force of diffusion, thereby increasing the diffusion range. Moreover, it is the oxygen dissolved in plasma that is more bioavailable to tissues. At 3ATA, hyperbaric oxygen increases the level of dissolved oxygen in the plasma from 0.3 to 6ml/dL to ensure that the amount of oxygen needed for metabolism is independent of the amount chemically bound to hemoglobin.
While there are no official guidelines to date supporting the use of hyperbaric oxygen to treat fibromyalgia patients, the first report on its use in fibromyalgia was in 2004. Since then, a large number of papers have been conducted to validate the effectiveness of hyperbaric oxygen as a treatment option for patients with fibromyalgia and to elucidate the molecular mechanisms by which hyperbaric oxygen can produce positive effects.
Hyperbaric oxygen represents a non-invasive potential treatment option because of its ability to reduce oxidative stress that occurs in hypoxic tissues. In fact, a large body of data showed a change in the pro-oxidation and antioxidant balance in fibromyalgia patients, characterized by reduced function of superoxide dismutase (SOD), nicotinamide adenine dinucleotide phosphate oxidase (NADPH), and catalase (CAT), which correlated strongly with the severity of pain and fatigue assessed by FIQR.
Hyperbaric oxygen can inactivate caspase3 and caspase9, increase the expression of bcl2 gene, and thus increase the apoptosis of regulatory cells. This finding suggests that the increased supply of oxygen produced by hyperbaric oxygen reduces mitochondrial apoptosis and protects mitochondrial function. In addition, in animal models, hyperbaric oxygen can reduce lipid peroxidation and pro-oxidation processes. Studies in animal models have shown that muscle tissue ischemia is a severe activator of nociceptive receptors in unmyelinated muscles and can promote central sensitization. Reduced oxygen supply in the muscle tissue of fibromyalgia patients affects structural and functional changes that in turn play a role in the sensitization of central and peripheral pain receptors, thereby altering central pain perception and processing. This finding also supports the therapeutic role that hyperbaric oxygen may play in these patients.
In addition, hyperbaric oxygen has anti-inflammatory effects, promotes neuroplasticity, optimizes mitochondrial function, and stimulates nitric oxide, which may reduce hyperalgesia and promote the release of endogenous opioids. In addition, Guggino et al. report how the immune system plays a role in the pathogenesis of fibromyalgia and outline the therapeutic effects of hyperbaric oxygen by describing changes in CD4T cell subsets that produce pro-inflammatory cytokines (IL-1RA, IL-6, IL-8). These results support hyperbaric oxygen as an effective, safe and rapid way to treat the various symptoms of fibromyalgia.
Criticism of this treatment has to do with the overproduction of oxygen free radicals, which may be responsible for excessive pro-oxidation reactions. In our clinical experience, oxidative stress resulting from therapeutic use in accordance with hyperbaric oxygen guidelines does not result in adverse reactions. One possible explanation is the so-called "high-oxygen-low oxygen paradox." Let's try to clarify what it means succinctly. Cellular respiration is a complex biochemical process, based on mitochondria, involved in the complete oxidation of glucose molecules to form carbon dioxide, water, and adenosine triphosphate (ATP) molecules. Low oxygen leads to reduced production of adenosine triphosphate. It is also one of the strongest inducers of gene expression, capable of influencing changes in metabolic structure, regenerative processes including angiogenesis, and stem cell mobilization, migration, and differentiation. Changes in oxygen levels in hyperoxic-hypoxic sensation are detected by chemoreceptors and are capable of inducing metabolic changes through molecular mechanisms. Even more interesting is that, at the cellular level, fluctuations in free oxygen are considered to be a reduction in oxygen supply, rather than a reduction in absolute oxygen values. In patients treated with hyperbaric oxygen, oxygen levels fluctuate, rising from 21% to 100% in the hyperbaric state before returning to base levels at the end of treatment. The adaptive response to repeated hyperoxy led to an up-regulation of scavenger (antioxidant) production, accompanied by an increase in ROS production. The return to physiological oxygenation levels (ambient air) is characterized by a low ROS/ scavenger ratio, which is related to the different half-lives of ROS and scavenger (the former has about half the half-life of the latter). This up-regulation of the scavenger can play a protective role by balancing the overproduction of oxygen radicals. Repeated exposure to hyperoxygen thus mimics hypoxic scenarios at the molecular level by triggering a transcriptional cascade of molecular effects induced by hyperbaric oxygen. So far, however, hyperbaric oxygen has produced positive results in several clinical trials, with an overall increase in nerve function affected by fibromyalgia
It is clear that the results of case reports are related to the reported personal experience and clearly cannot be considered to reproduce with absolute reliability across large populations. Similarly, the follow-up data for these patients extended to 6 months in most of the work, which may also be a limit to the duration of judging the beneficial effects produced by hyperbaric oxygen. In addition, the various works on this topic do not use the same scheme, but differ in terms of exposure time and work pressure used, which may constitute further bias. From this perspective, one has to take into account the great difficulty that researchers manage to generate clinical trials that recruit large numbers of patients, which is unfortunately related to several factors, such as the lack of knowledge of the indications for hyperbaric oxygen by many physicians, their low level of information on the powerful auxiliary role that hyperbaric oxygen can play in treating such patients, the rare geographical distribution of hyperbaric chambers, and the lack of information on the potential role of hyperbaric oxygen in treating such patients. And the difficulties associated with the economic costs required to manage hyperbaric oxygen therapy, especially for a pathology like fibromyalgia, which to date has no guideline support.
With the end of hyperbaric oxygen therapy, the patient has been following the multistructural therapy proposed by the rheumatology department and reports that she feels fine, no longer reporting changes in the psycho-neuro-sensory and functional areas that severely impaired her quality of life prior to hyperbaric oxygen therapy.
conclusion
We report our experience in the treatment of a fibromyalgia patient with hyperbaric oxygen. Fibromyalgia is a very deadly condition that often afflicts young people. The quality of life of these patients is compromised, with serious consequences for the public economy.
Hyperbaric oxygen is a safe trial treatment for fibromyalgia because it improves the quality of life for these patients and reduces its economic impact on society. Further research is needed to improve our understanding of the potential mechanism of action of hyperbaric oxygen and clarify its role in treating these chronic conditions. Barometric medicine represents a direction that still offers great scientific exploration. Perhaps, improving communication between different hyperbaric centers could be the first step toward creating a truly powerful hyperbaric medicine network capable of improving how we treat patients.
1.The hyperbaric oxygen pressure in the treatment of fibromyalgia patients in this literature is 2.4ATA. Xiaobian believes that fibromyalgia is mainly caused by problems in the metabolism of the muscle system. Based on the theoretical time of saturation and desaturation of different tissues, hyperbaric oxygen treatment pressure is deduced. Treatment programs can be given with higher pressure (but not more than 2.5ATA, increasing side effects) and appropriate extension of oxygen inhalation time (such as full oxygen inhalation, increasing the time or number of stable oxygen inhalation, but intermittent air inhalation is required for stable pressure).
2.for after hyperbaric oxygen treatment, has been significantly improved, or in the chronic or stable period, can be given 2.0ATA conventional treatment program. For the total number of treatments, 40 treatments are required according to the patient's needs, such as the need to improve sleep quality. According to the patient's nutritional status, physical condition, whether there is weakness, etc., decide the appropriate rest between treatment courses.
3.For the hyperbaric oxygen treatment of 2.4ATA patients, according to the theory, it is necessary to take a step decompression program when 2.25ATA is above to reduce the risk of decompression sickness in the cabin. In addition, focus on the cabin crew (whether it is patients or medical staff, in the high pressure air, so in the pressure and pressure regulation stage has been in a nitrogen saturation state), in addition to the step decompression program, you can also take the pressure regulation stage and decompression stage oxygen.
4.As a hyperbaric oxygen medical staff, you can form an MDT team together with rehabilitation, rheumatology, psychology, neurology and psychology teams to conduct comprehensive treatment, and also conduct basic or clinical research on hyperbaric oxygen therapy in this field to enrich the research content and mechanism of hyperbaric oxygen therapy for fibromyalgia.
5.learn to use good publicity good hyperbaric oxygen, we work together and hand in hand.